There are few ECG features that are unique to junctional rhythms, so identification of junctional rhythms should focus on ruling out atrial and ventricular rhythms. When attempting to confirm or rule out a junctional rhythm, remember that junctional rhythms are always perfectly regular. No exceptions! But note that atrial and ventricular rhythms can also be perfectly regular. Junctional rhythms can also be either narrow or wide-complex, so we need understanding of more variables to help us confidently identify junctional rhythms.
As a side-note, we should probably mention that junctional rhythms can appear irregular if they are interspersed with premature atrial and ventricular beats, or if they are transitioning back-and-forth between an atrial or ventricular rhythm and the junctional rhythm, but remember, ignoring rhythm transitions and premature beats, the junctional rhythm itself will always be perfectly regular.
P-R intervals in junctional rhythms are always less than 0.12 seconds (if the P-wave even exists). Please don't merely memorize this, understand why! The P-R interval must be less than 0.12 in a junctional rhythm because it always takes more than 0.12 seconds for an electrical impulse to travel from the atria to the ventricles through the AV node, so if the space between the P wave and the QRS complex is less than 0.12, then the impulse causing the ventricular depolarization can't be coming from the atria! Ergo, it must either be a ventricular rhythm or a junctional rhythm. A narrow-complex would allow you to further rule out ventricular rhythms, leaving only a junctional rhythm as a possibility.
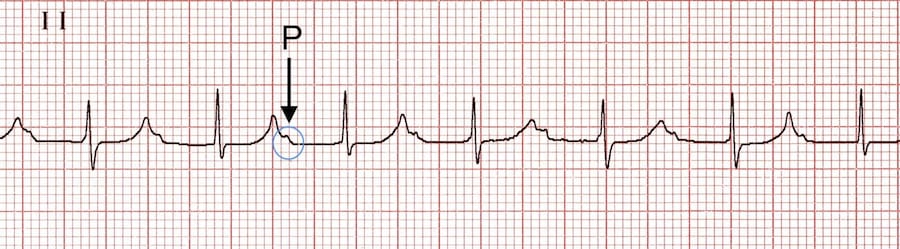
But if the depolarization impulse is not coming from the atria, then why is there often still a P-wave associated with the QRS complex? This is often because of something called "retrograde depolarization." Signals from the junction and ventricles can go backwards up the conduction system and depolarize the atrium, causing a P-wave. P-waves caused by this retrograde depolirization are often (but not always) inverted in the inferior leads like lead II because the electricity is travelling in the opposite direction (bottom-to-top instead of top-to-bottom) as the atrium depolarizes, resulting in an upside-down P-wave. It's important to understand that depolarization of the AV node and conduction system itself doesn't register at all on the ECG strip; the fibers of the conduction system are simply not enough tissue. You don't see anything on the ECG strip until the electricity exits the conduction system and starts depolarizing muscle tissue. There's a lot more cells in the muscle than there are in the conduction system, hence a lot more electricity moving around. If an impulse originates in the junction and reaches the atrium before the ventricles, the P-wave will appear in front of the QRS complex. If that same impulse arrives at the ventricles before it arrives at the atrium, the P-wave will appear either after the QRS complex, or it will be buried inside the QRS complex if the QRS complex is wide enough to eat the P-wave.
Don't use inverted P-waves to identify junctional rhythms. Inverted (upside-down) P waves are neither specific nor 100% sensitive to junctional rhythms. Inverted P-waves (in the inferior leads) are often produced by retrograde depolarization from both junctional and ventricular rhythms, but retrograde depolarization can also produce upright P-waves, and even some impulses originating in the atrium (for example an ectopic focus low in the atrium) can produce upside-down P-waves. Inverted P-waves are a good clue that you may be looking at a junctional rhythm, but they can't be used to confirm or rule out anything. On the other hand, when PR intervals are abnormally short (less than 0.12), or the P-waves are consistently in the "wrong" location (after the QRS or buried inside the QRS), and the number of P-waves matches the number of QRS complexes, then that is conclusive evidence that you're looking at either a junctional or ventricular rhythm. And if the rhythm is narrow-complex and has a PR interval less than 0.12 (or is narrow-complex and matches the conditions described above), then that's conclusive evidence that you're looking at a junctional rhythm.
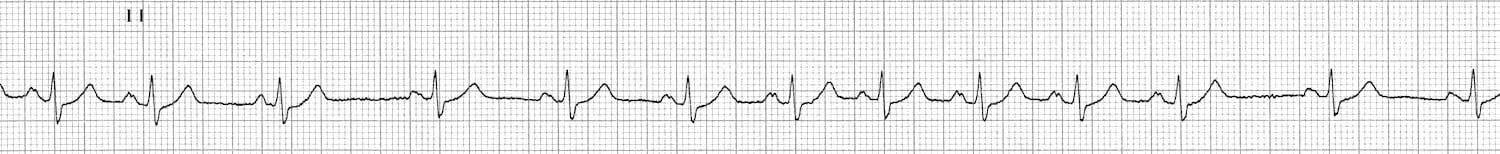
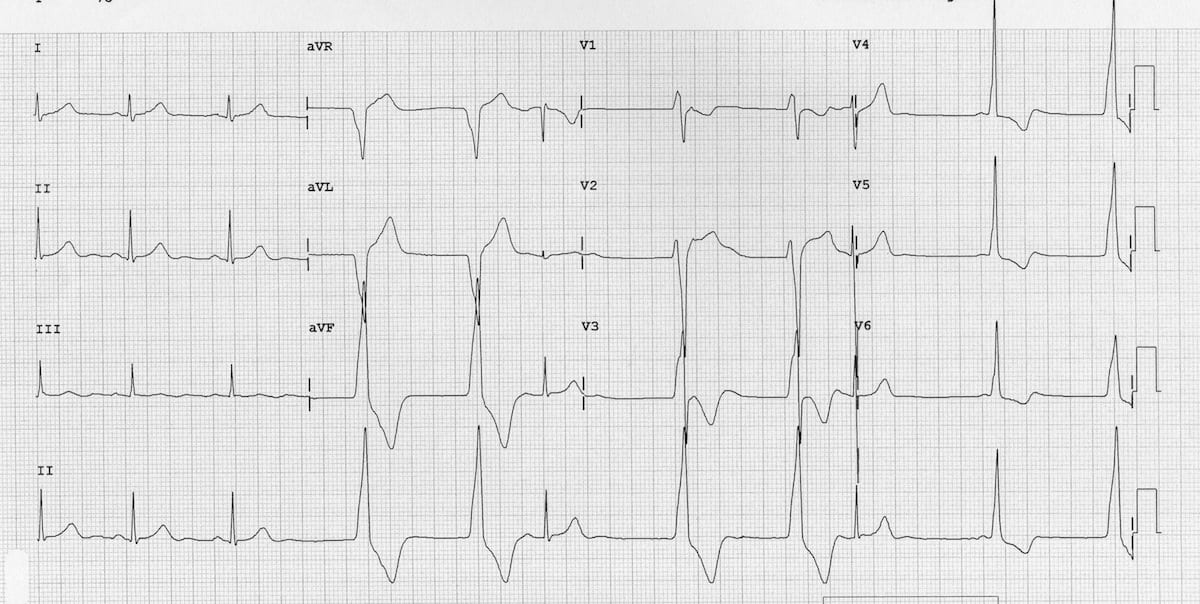
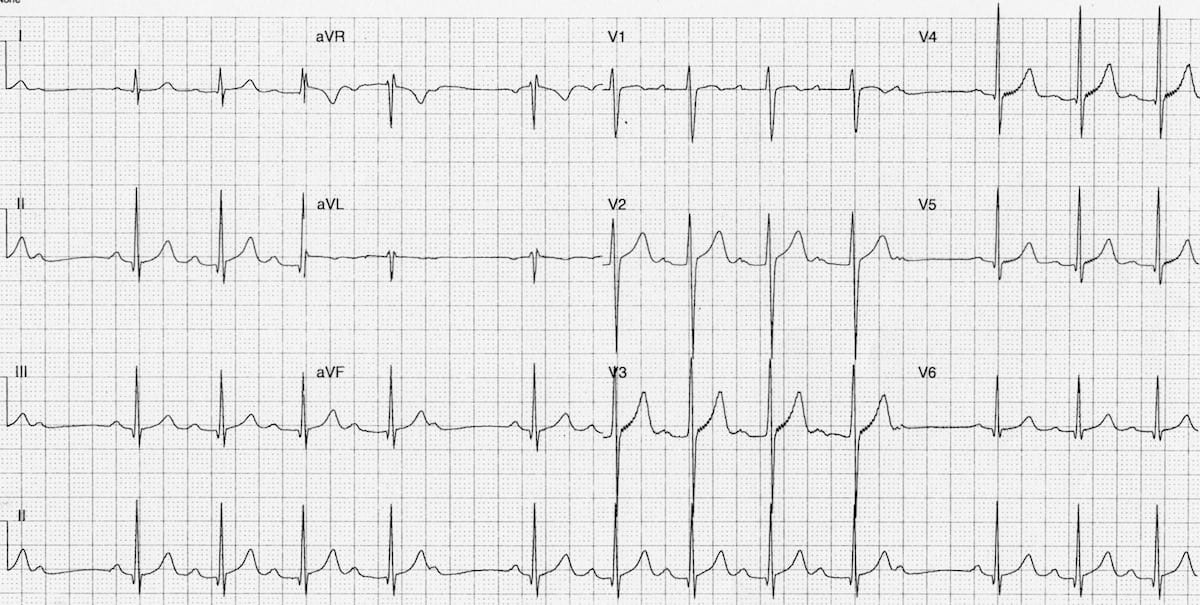
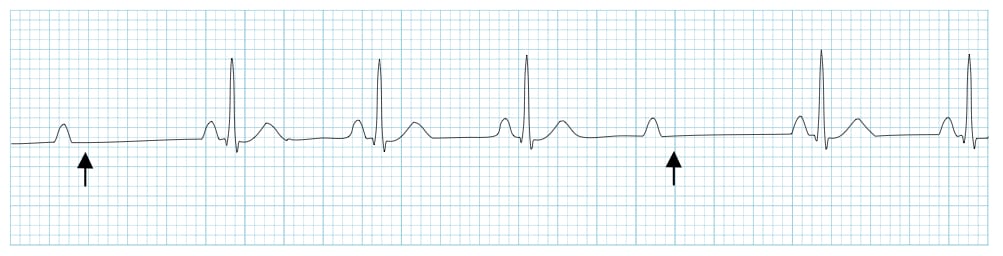
Here's an interesting example:

This is a lewis lead (increases amplitude of P-waves for easier rhythm identification) of a patient that I took care of after a mitral valve replacement. I initially ran this particular rhythm by several cardiologists and got several completely different identifications for this rhythm.
The atrial complexes are perfectly regular and monomorphic, and they appear to lack the "sawtooth" shape characteristic of atrial flutter. The R-R spacing is also perfectly regular, with a HR of 77. At first glance, this appears to be a simple case of atrial tachycardia with 4-1 conduction. But something unusual is going on here. Can you spot the anomaly?
Notice that the PR intervals are completely random. The P waves appear to have no relationship to the QRS complexes. This is not strange in-and-of-itself; there are plenty of irregular atrial arrhythmias that produce irregular PR intervals, but if the ventricles are following the atria, then an irregular impulse must produce an irregular rhythm, and if a regular impulse is producing a regular rhythm, then the PR intervals must be regular. The fact that the R-R intervals remain perfectly regular here, despite the PR intervals being all over the place, tells us that the P waves are not linked to the QRS complexes... which means that the ventricular rhythm is not listening to the atrial rhythm. Recall that the heart doesn't really have one rhythm; it has two (atrial and ventricular). Those two rhythms are usually in synchrony, but here is a case where that synchrony has been broken.
But if the rhythm in the ventricles here (the QRS complexes) is not coming from the atrium, where is it coming from? Well, the QRS complexes are narrow, which means it's not a ventricular rhythm. This is an accelerated junctional rhythm, with a background of atrial tachycardia.
Why aren't any of the atrial impulses getting through to the ventricles here? It's because this patient had a mitral valve replacement. The mitral valve is very close to the AV node. Inflammation of the AV node can impair it, resulting in an AV node that is easily fatigued. When this patient entered an atrial tachycardia, those rapid impulses from the atrium were simply too much for the patient's inflamed and tired AV node, and the AV node stopped transmitting the impulses. At that point the conduction system tissue a little farther down the track, either in the AV node or somewhere in the bundle of His, lacking any input from the atria and irritated by the inflammation from the surgery, produced an accelerated escape rhythm.
Now, I know what you're thinking: "Zero conduction through the AV node? That sounds like a 3° AV block to me." That's certainly what I thought, but the electrophysiologists that I spoke to regarding this rhythm informed me that complete blockage of the AV node that is due to fatigue caused by rapid atrial impulses is not a 3° AV block. Unfortunately they were unable to offer me an alternative definition for this manner of transient complete AV block (perhaps such a circumstance is rare enough that there is no commonly-accepted definition). I'm no electrophysiologist so I yield to their authority, but suffice to say, this is functionally identical to a 3° AV block.
In case you're wondering how we knew this block was rate-dependent, I actually watched this patient transition multiple times between this rhythm and sinus rhythm with a 2° type-1 AV block. Whenever the patient's atria exited Afib and returned to NSR, the AV node would resume transmission of impulses and the atrium would recapture the ventricles.
One big takaway here is that AV blocks can be rate-dependent just like bundle branch blocks. This is also a perfect example of how simple definitions and memorization of ECG patterns in textbooks can fail you, and how a basic understanding of the mechanics of the conduction system can elucidate what is happening in a patient's heart and the clinical implications, even in edge cases where professionals are unable to agree on a definition for what's happening!
To summarize some important rules for identifying junctional rhythms:
- Junctional rhythms are always perfectly regular (not counting premature beats & rhythm transitions).
- Neither P-wave morphology nor width of the QRS complex in isolation can be used to confirm or rule out a junctional rhythm.
- Junctional rhythms may or may not have associated P-waves, but if P-waves are present and associated with the QRS complexes then they will probably be inverted in the inferior leads, and they will never have a PR interval greater than 0.12.
- If a 3° AV block is present, a junctional rhythm can present with a background of any atrial rhythm. For example, a heart can be in Aflutter and a junctional rhythm at the same time.
- Because there are few ECG features that are unique to junctional rhythms, identification of junctional rhythms should focus on ruling out atrial and ventricular rhythms.